Health care is at a true tipping point. Throughout my three decades in the industry—across UnitedHealth Group, Walgreens, Magellan Health, and now MOBE— I’ve seen waves of change (remember when PPO plans were new and revolutionary?). Yet, here we are, 30 years later, still patching up the same systems and expecting different results. Even with cost trends at 11% and rising, people aren’t getting healthier. Health care isn’t getting better. It’s time for something new.
Today, half of U.S. adults now live with at least two chronic conditions (that’s a 142% increase since 2001). Among young adults aged 18–34, the rate of multichronicity has jumped 25% since 2013. I’ve seen the landscape change where once the typical member or employee maybe managed a single chronic condition. Now, the average among those we support has four.
This health crisis is out of control, and our industry is scrambling to keep up. It feels like there might not be a way back from this, but if we invest in proactive intervention strategies now, hopefully we can look back at this pivotal moment as the one when we turned things around.
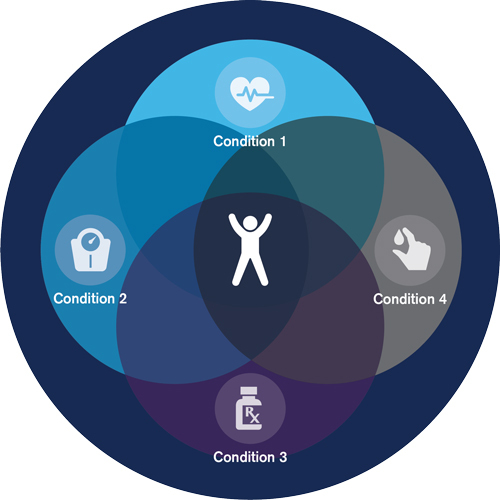
Managing multiple conditions—diabetes, arthritis, hypertension, insomnia, the list goes on—brings an overwhelming level of complexity that’s hard to overstate. But the challenge extends beyond just managing symptoms. It’s about the interactions between conditions, the side effects of multiple medications and supplements, and how an everyday cold can spiral into something far more serious and expensive.
Now this person is too sick to go to work; they’re having side effects from all the medications they’re taking, including the over-the-counters from the cold. They’re depressed, losing sleep, and their relationships are suffering. They’re so stuck between being overwhelmed and feeling terrible that they can’t get off the couch.
We have forgotten about the basics of health; the proactive nature of getting lifestyle right. People need to get their meds handled. They need to move their bodies. They need to get better sleep and eat well. They need to feel good both physically and mentally. We have to move from sick care to real, whole health care.
Let’s put this further in perspective. Imagine a high-risk diabetic managing type 2 diabetes along with hypertension, depression, and cardiovascular disease. He sees four different specialists on opposite sides of town who each prescribe him medications after 10-minute visits. Meanwhile, he takes a supplement and a few herbal medicines his cousin swears by and gets health advice from ChatGPT, searching online, and social media. None of his providers see the whole picture, and no one is helping him connect the dots.
Employee wellness and clinical programs might be available through employers, but time and energy are in short supply. Communication is fragmented, outreach feels nagging, and confusion leads to disengagement. Stress and depression make management harder, compounding clinical and life challenges.
This story isn’t unique. Complex health profiles translate into overutilization: more frequent ER visits, longer hospital stays, and rising costs point to not just unmanaged conditions but unmet mental, emotional, and social needs. People need guidance and a new kind of support.
For employers, this challenge goes far beyond the doctor’s office:
Our biggest flaw is how we treat conditions. After diagnosis, the first line of treatment is to improve lifestyle habits like getting more sleep, eating better, working on mental health, and getting exercise. Providers expect little follow-through, for us to fail on our own, so scripts are written and the cycle continues.
When health care cost trend reached one of the first tipping points I’ve seen in my career, employers and payers found single-condition solutions as the most effective strategy for both outcomes and cost: add a new diabetes app here, an MSK benefit here, and a mental health program there.
Today, there are over 400 point solutions, yet most ignore the complex web of real cost drivers: the connections between mental, physical, and social health. Neither providers nor care managers have or take the time to walk patients through their complicated health pictures, coordinating between specialists and tracking conflicting advice. One only has to look at care manager average handle time (AHT) to know whether a program has a chance or not. As program engagement drops and confusion grows, gaps in care widen—and we find ourselves stuck amidst double-digit cost trends.
Health care is extraordinarily complex. A friend who managed worldwide flight operations at a large airline once told me that safely moving thousands of planes, passengers, and their bags wasn’t nearly as complicated as the U.S. health care system. We have a big problem on our hands.
While we can’t change things overnight, we can start making investments now. The answer to bringing these explosive costs down isn’t cutting programs or administration fees. We need to start with how we change the mindset and motivate those with multiple chronic conditions.
Here’s how leaders can instigate change:
This is our moment to lead boldly. Health plans and large employers are already consolidating vendors to save on costs, but that alone won’t get to the root of the problem. We need to address the “sick care” mentality and think about getting people back to lifestyle basics. Because if we think chronicity is bad now, it’s going to double in the next five years.
We can keep reacting to increasing costs and people getting sicker and watch the system buckle, or we can address real, whole health. The leaders who step into this new era looking to change the way we treat health care—by adopting a biopsychosocial, whole-person approach—will build stronger, healthier, and more engaged teams.